
Diet, Lifestyle, and Prevention: Breast Health Tips for Indian Women
Learn how diet, lifestyle changes, and early habits support the prevention of breast cancer in Indian women. Practical breast health tips from Panacea Clinic.
As women, we notice changes in our breasts and get worried about them. With so much information available online, we try to diagnose ourselves and the first thing that comes to our mind is ‘breast cancer’.
As a breast oncologist in Nagpur, I see patients every day who walk into my clinic worried, and I completely understand their concerns. But please understand that every breast change does not mean cancer.
The statistics are sobering but also empowering: in 2021, 2.3 million women were diagnosed with breast cancer globally[1].
But here’s the hopeful part – when caught early, the five-year survival rate is an incredible 99%. When detected late? Just 27%[2].
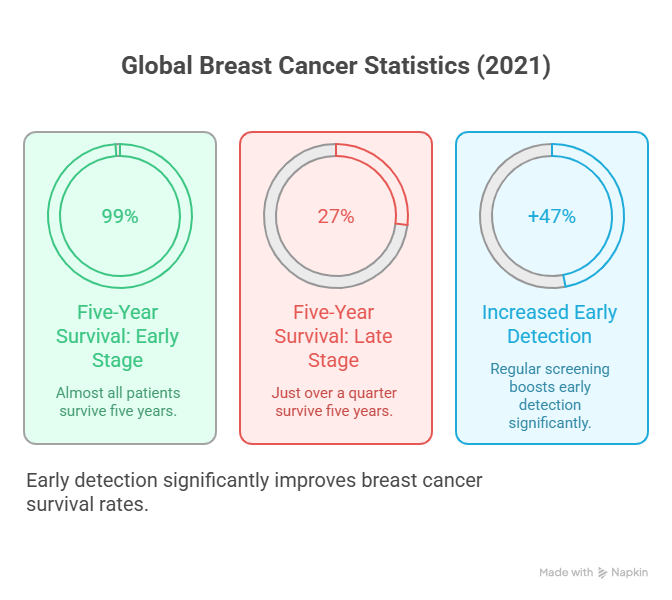
That 72-point difference is exactly why knowing when to worry matters so much.
In India, too, breast cancer cases are steadily rising. According to the Global Cancer Observatory (WHO, 2024), the number of new breast cancer cases among Indian women is expected to increase from 192,000 in 2022 to 209,000 in 2025, which is an alarming 9% rise in just three years.
This upward trend reflects not only changing lifestyles and delayed motherhood but also improved awareness and screening. It’s a reminder that early detection isn’t just life-saving globally, it’s becoming increasingly crucial for Indian women right now.

This blog will help you understand the exact signs and symptoms that indicate when you need to consult a doctor or simply relax.
Do your breasts feel lumpy, tender, or full, especially before your period? You’re not alone – up to 70% of women experience this[3]. It’s called fibrocystic breast changes, and it’s so common that we barely consider it a disease anymore.
Your breast tissue responds to hormonal fluctuations throughout your menstrual cycle. Estrogen peaks around the time of ovulation, causing the breast ducts to enlarge.
Then, progesterone rises, causing the milk glands to swell. When your period starts and your hormones drop, the discomfort typically fades.
Sometimes the solution is simpler than you think:
Suppose you’ve previously been diagnosed with fibroadenomas (smooth, movable lumps) or simple cysts (fluid-filled sacs), and they haven’t changed in size, shape, or texture. In that case, you can generally relax – but do keep your monitoring appointments[8].
Pain that comes and goes with your menstrual cycle, typically starting 7-14 days before your period and improving once menstruation begins, is usually benign. Studies show that 60% of cyclical breast pain resolves spontaneously within a few years[9].
Now for the red flags. These symptoms need prompt evaluation:
This is the most common presenting symptom of breast cancer[10]. While 80% of breast lumps are benign, a thorough evaluation is necessary to confirm the diagnosis [11].
Your breast skin tells important stories. See me right away if you notice:
Redness or warmth: This could be inflammatory breast cancer, a rare but aggressive form that looks like an infection. If antibiotics don’t help within 2-3 days, further evaluation is needed [12].
Dimpling or puckering: When tumours attach to underlying tissue, they can pull the skin inward. This orange-peel texture (known as “peau d’orange”) requires immediate assessment. [13]
Scaling or crusting on the nipple: This could be a sign of Paget’s disease, a rare form of cancer that affects the nipple area [14].
Bloody or clear discharge: Especially concerning if it’s spontaneous (without squeezing), from one breast only, or from a single duct. While often caused by benign conditions, 5-21% of cases are cancer[15].
New nipple inversion: If a nipple that previously pointed out suddenly turns inward, a tumour may be pulling it. This is different from nipples that have always been inverted – those are considered normal variants [16].
Sudden, unexplained changes in how your breasts look deserve attention. One breast becoming noticeably larger or smaller, or a visible distortion in the breast contour, could indicate underlying problems. [17]
While most breast pain isn’t cancer-related, persistent pain that doesn’t follow your cycle, is localised to one spot, and especially pain accompanied by lumps or skin changes needs evaluation[18].
Breast pain accompanied by fever, redness, swelling, and warmth may indicate mastitis – a breast infection that requires antibiotics. Don’t wait on this, as untreated infections can form abscesses that require drainage [19].
When you come to see me with concerns, we’re accomplishing three critical things:
Ruling out cancer: Early-stage breast cancer offers treatment options that preserve your breast, often avoid chemotherapy, and offer a 99% survival rate[2].
Diagnosing other conditions: Infections, injuries, and benign conditions also require proper treatment.
Providing peace of mind: Knowing definitively that a lump is benign allows you to sleep at night.
Beyond watching for symptoms, regular screening catches cancers before you can feel them.
Mammography recommendations:
Research shows mammography screening reduces breast cancer deaths by about 20%[21].
High-risk women (BRCA mutations, strong family history, chest radiation before age 30) need enhanced screening starting earlier, often including annual MRI[22].
You can’t control your genetics, but you can influence many risk factors:
Exercise regularly: Studies show that 150 minutes of moderate exercise per week reduces the risk of breast cancer by 12-21%[23].
Maintain a healthy weight: Post-menopausal obesity increases risk because fat tissue produces estrogen. Losing even 5% of body weight reduces risk by 12%[24].
Limit alcohol: Each daily drink increases risk by 7-10%. If you’re high-risk, consider avoiding alcohol altogether[25].
Don’t smoke: Smoking increases breast cancer risk, particularly if you started before your first pregnancy[26].
Breastfeed if possible: Each 12 months of breastfeeding reduces risk by 4.3%[27].
“If breast cancer doesn’t run in my family, I’m safe.” Wrong. About 85% of women with breast cancer have NO family history[28].
“Underwire bras cause cancer.” Completely false. No scientific evidence supports this[29].
“I’m too young to worry.” While risk increases with age, breast cancer does occur in younger women – and tends to be more aggressive[30].
“A negative mammogram means I definitely don’t have cancer.” Mammography misses about 13% of cancers, which is why maintaining breast awareness is important [31].
After years in practice, I’ve learned that informed, proactive women do best with breast health. They don’t ignore symptoms, but they don’t catastrophize every change either.
That 99% early-stage survival rate versus 27% late-stage survival represents lives saved and futures that continue. The key? Early detection through awareness, prompt evaluation, and appropriate screening.
Most breast changes are benign, but getting them evaluated is how we catch the ones that aren’t – when they’re most treatable. Please don’t hesitate to reach out with any concerns. Your health is worth protecting, your concerns are worth addressing, and your peace of mind matters.
With warmth and dedication to your health,

Learn how diet, lifestyle changes, and early habits support the prevention of breast cancer in Indian women. Practical breast health tips from Panacea Clinic.

Namaste, Last Tuesday, I met Priya in my clinic. She’s 32, works in IT, newly married, and was holding a report that had just turned

Yesterday I was passing near a college and I saw a group of students vaping near the campus. Probably one of them was reluctant to

As women, we notice changes in our breasts and get worried about them. With so much information available online, we try to diagnose ourselves and

Namaste,I’m Dr. Arundhati Marathe Lote, a breast cancer surgeon. But before anything else, I’m a woman, just like you. And today, I want to talk
As a chest specialist practising in Nagpur for over twelve years, I have had the privilege of helping hundreds of families understand pulmonary fibrosis treatment.