Breast Screenings in Nagpur – Early Detection, Better Outcomes.

Quick Enquiry
What is Breast Screening?
Breast screening is a simple, preventive health check that helps find changes in breast tissue, sometimes even before symptoms appear.
Think of it as a gentle, proactive step toward protecting your health.
We understand that just the thought of screening can bring a wave of emotions like nervousness, uncertainty, or even fear. That’s completely natural. But know this: breast screening is not about expecting the worst. It’s about giving yourself the best chance, the chance to catch something early, when it’s often most treatable.
Why is Breast Screening Important?
Breast screening isn’t just a medical test. It’s a way to gently stay ahead of something that often shows no signs in its early stages. Many breast cancers start silently, without any pain, lumps, or visible symptoms. Screening helps spot changes in breast tissue before they become noticeable or serious.
Research has shown that finding breast cancer early can lead to more effective treatment and significantly better outcomes. In fact, when detected at an early stage, the 5-year survival rate can be as high as 99% (American Cancer Society).
Several global studies, including those in Sweden and the U.S., have also confirmed that regular breast screenings reduce the risk of dying from breast cancer by up to 40%.
But beyond the numbers, screening gives you peace of mind. It lets you know what’s happening inside your body, even when everything feels fine on the outside. And if something is found, it’s often early enough to act on it with confidence.
You’re not doing this because something is wrong. You’re doing it because your health matters. Because prevention is power.
Who Should Consider Breast Screening?
Every woman deserves to feel informed and in control of her health. While breast screening isn’t one-size-fits-all, here’s some guidance to help you understand when it might be right for you.
For most women:
Many global and national health organisations recommend starting regular mammograms if you’re 40 years or older. The frequency, whether yearly or every two years, can depend on your personal risk factors and should be discussed with your doctor.
For women at higher risk:
You may benefit from earlier or more frequent screenings if you:
Have a family history of breast or ovarian cancer (especially in a mother, sister, or daughter)
Have a known BRCA1 or BRCA2 gene mutation.
Received radiation therapy to the chest before age 30
Have certain non-cancerous breast conditions or a strong personal health history
Your age, history, concerns, and comfort all matter. That’s why we encourage an open, personalised conversation to determine the best screening plan for you, not just based on numbers, but on what gives you confidence and peace of mind.
You’re not alone in this journey. We’re here to help you make informed choices at every step.
Types of Breast Screening Tests
When it comes to breast screening, you have options. The right test depends on your age, risk level, and comfort, but knowing what each involves can help you feel more prepared and in control.
Here are the most common types of screening tests used to check breast health:
Clinical Breast Exam (CBE)
This is a hands-on examination performed by a trained healthcare provider to detect lumps or other abnormalities. It’s often done as part of your routine health check-up.
CBE is recommended once a year for all women aged 20 years and above.
Breast Ultrasound
Used alongside a mammogram, especially for women with dense breasts or when something unusual is found. It uses sound waves (not radiation) to create detailed images, hence it is absolutely safe.
We might advise against a mammogram and recommend only a breast ultrasound based on your age, risk factors, and family history.
It is recommended for women under the age of 40.
Mammogram (2D or 3D Digital Mammography)
The most commonly used screening tool is a mammogram, a low-dose X-ray that captures detailed images of breast tissue.
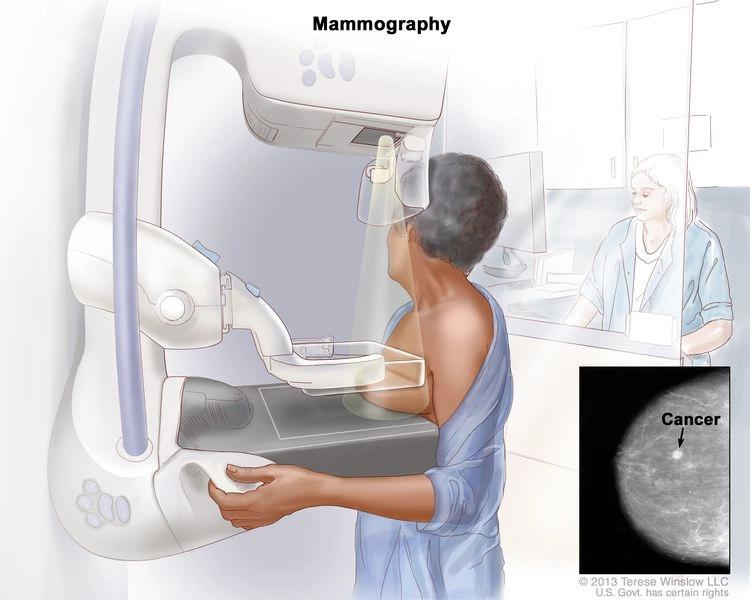
- It can detect lumps or changes long before you can feel them.
- It can detect cancers even before lumps are formed.
- 3D mammography (also called tomosynthesis) offers even more explicit images, especially useful for women with dense breast tissue.
- The process is quick, usually taking under 15 minutes, and is not painful at all.
- The radiation exposure is minimal and not harmful if done at correct intervals as per your doctor’s advice.
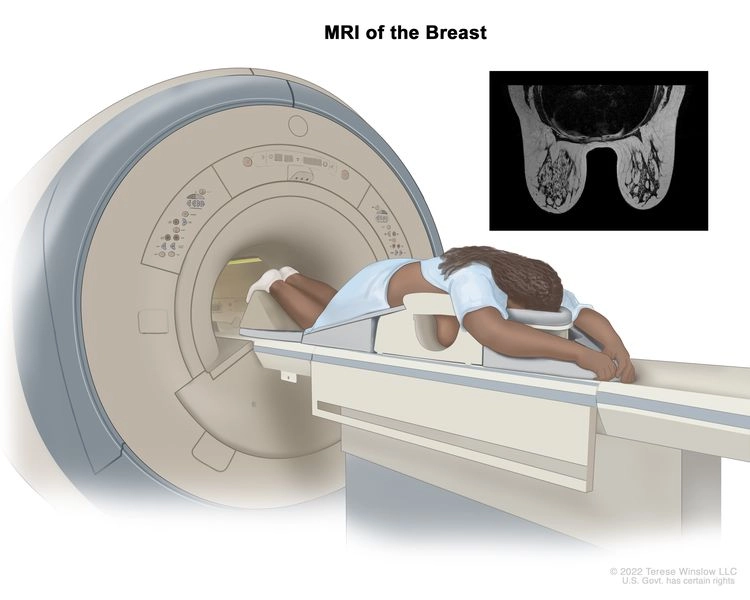
Breast MRI (Magnetic Resonance Imaging)
Recommended for high-risk women, such as those with BRCA gene mutations or a strong family history. MRI uses magnets and radio waves to produce very detailed breast images.
Self-Breast Exam (SBE)
Your hands can be your first alert system.
This simple, monthly check helps you become familiar with how your breasts normally look and feel, so you’re more likely to notice changes between regular screenings.
It’s the strongest tool any woman can have, and it’s completely free.
Here’s how to do it:
- Look in the mirror: With arms by your side, then overhead, look for any skin changes, swelling, or nipple changes.
- Feel your breasts: Use the pads of your fingers in circular motions, covering the entire breast and underarm area. Try it in the shower or lying down.
- Repeat monthly: Ideally, after your period ends (or pick a fixed day if you're postmenopausal).
If you ever notice a new lump, thickening, or any other change, don’t panic; instead, reach out to your doctor.
Not sure which test is right for you?
That’s okay. We will guide you based on your health history, age, and comfort. The most important thing is to begin the conversation and take that first step.
Breast screening isn’t about fear. It’s about awareness, clarity, and confidence in your body’s story.
What to Expect During Your Screening
We know that coming in for a breast screening, whether it’s your first time or your fifth, can feel overwhelming. But knowing what to expect can ease that anxiety and help you feel more in control.
Depending on your risk level and your doctor’s recommendation, your screening may include a mammogram, a breast MRI, or both. Here’s what you need to know:
If You’re Getting a Mammogram
- You’ll be asked to undress from the waist up (a gown is provided) and stand in front of a mammography machine.
- One breast is placed between two soft, flat plates, which gently compress the tissue for a few seconds while the image is taken.
- You may feel some pressure, but it’s brief and usually well tolerated.
- The full procedure takes around 10–15 minutes.
- Most women are able to return to their normal day right after.
Avoid using deodorant or powder before the test, as they can affect the images. If your breasts feel tender before your period, consider scheduling the test for a different time.
If You’re Getting a Breast MRI
- Breast MRI is typically recommended for high-risk individuals or when an unusual finding is detected in a mammogram.
- You’ll lie face down on a cushioned table with openings for your breasts. The table then slides into a scanner.
- The machine uses magnets and radio waves to create detailed images; no radiation is involved.
- The scan typically takes 30 to 45 minutes, and you’ll need to remain still during this time.
- Some patients receive a contrast dye through a vein for clearer images. Your doctor will guide you in this process.
The MRI machine can be noisy, but you’ll be given earplugs or headphones. Talk to your care team if you feel claustrophobic; they’ll help you feel at ease.
Your Comfort Comes First
Regardless of the type of test, our team is committed to ensuring you feel safe, respected, and informed. You can always ask questions or take a pause during the process. Once your screening is complete, your doctor will explain the results in simple, clear language.
Because this isn’t just about detecting problems but about protecting your peace of mind. One small step today can give you the clarity and confidence to move forward tomorrow.
How Often Should I Get Screened?
There’s no one-size-fits-all answer.
The frequency of breast screening you need depends on your age, personal health history, family history, and overall risk factors. The best screening plan is tailored to you.
Here’s a general guide:
For most women with average risk:
- Ages 40–44: You can choose to begin yearly mammograms if you wish to start early.
- Ages 45–54: Mammograms are usually recommended once a year.
- Ages 55 and older: Depending on your doctor's advice and your comfort level, you may continue with yearly mammograms or switch to every other year.
For women at higher risk (e.g., BRCA gene mutation, strong family history, or past chest radiation):
- Screening may start earlier than age 40.
- Doctors may recommend both a mammogram and a breast MRI for annual screening.
- You’ll receive a custom plan after discussing your full medical history.
Results and What They Mean
Waiting for test results can be a stressful experience. But knowing what the results mean (and what they don’t mean) can bring clarity and comfort.
Here’s what to expect:
If your results are normal:
- That’s great news.
- It simply means no signs of concern were found in your breast tissue.
- You’ll continue with routine screenings, as recommended by your doctor, typically every 1–2 years.
If your results are unclear or show something unusual:
- Don’t panic.
- An “abnormal” result doesn’t mean you have cancer; it means that the images showed something that needs a closer look.
- Your doctor may recommend additional tests, such as a diagnostic mammogram, ultrasound, or MRI, to provide more clarity.
If further testing is recommended:
- These follow-ups help your doctor understand the nature of the changes, whether it's a benign (non-cancerous) condition, such as a cyst, or something that requires a core-needle or Tru-Cut biopsy.
What you should know:
- You’ll be informed about your results promptly.
- Your doctor will explain everything clearly, answer your questions, and guide you step by step.
- You won’t face anything alone; we’re here to support you with empathy, privacy, and expert care.
Getting screened is a sign of strength, not fear. Whatever the outcome, you’ve already taken an empowering step toward protecting your health.
Common Myths About Breast Screening
Breast screening can feel intimidating, especially when misinformation creates confusion or fear.
Truth: Most breast cancers found through screening show no symptoms at all. That’s why screening is so important; it helps catch changes before you feel or notice anything.
Truth: While you may feel slight pressure, it lasts only a few seconds. Most women describe it as uncomfortable rather than painful. And our team is here to ensure you’re as comfortable and supported as possible.
Truth: Not at all. Abnormal results simply mean that something unusual was observed, and further tests are needed for clarity. In most cases, the findings turn out to be non-cancerous (like cysts or benign lumps).
Truth: While the risk increases with age, breast screening can begin as early as 40, or earlier if you’re at higher risk. Your doctor can help create a plan that fits you.
Truth: A healthy lifestyle definitely supports your overall well-being, but it doesn’t eliminate risk. Breast cancer can affect anyone, regardless of lifestyle.
Screening isn’t about expecting bad news but about being proactive, informed, and empowered. The more you know, the more confident you’ll feel in taking care of your health.